Search
- Page Path
- HOME > Search
- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Association between the Diabetes Drug Cost and Cardiovascular Events and Death in Korea: A National Health Insurance Service Database Analysis
- Seung Min Chung, Ji-In Lee, Eugene Han, Hyun-Ae Seo, Eonju Jeon, Hye Soon Kim, Ji Sung Yoon
- Endocrinol Metab. 2022;37(5):759-769. Published online October 5, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1515
- 3,182 View
- 192 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study aimed to investigate the long-term effects of diabetes drug costs on cardiovascular (CV) events and death.
Methods
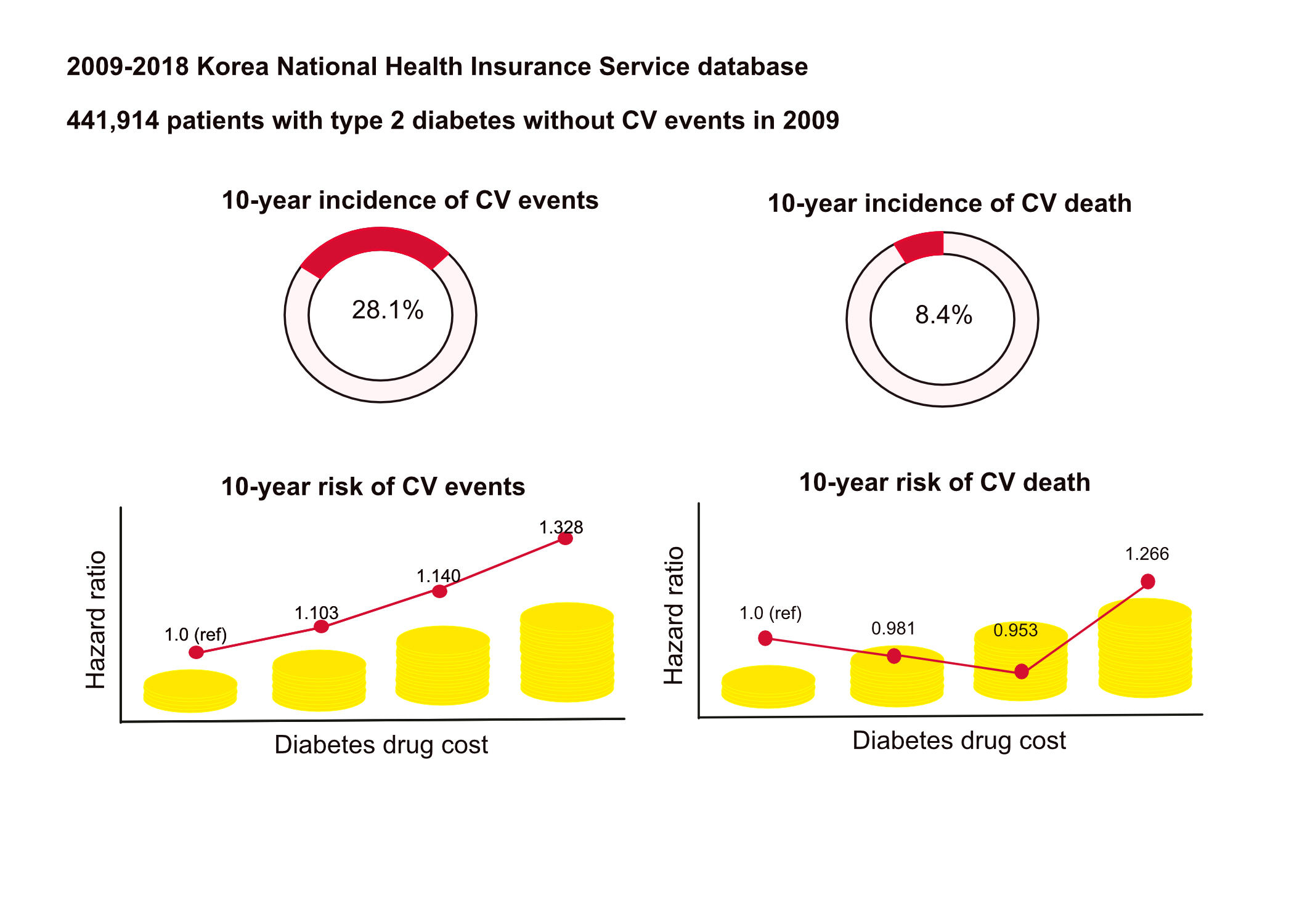
This retrospective observational study used data from 2009 to 2018 from the National Health Insurance in Korea. Among the patients with type 2 diabetes, those taking antidiabetic drugs and who did not have CV events until 2009 were included. Patients were divided into quartiles (Q1 [lowest]–4 [highest]) according to the 2009 diabetes drug cost. In addition, the 10-year incidences of CV events (non-fatal myocardial infarction, stroke, hospitalization for heart failure, and coronary revascularization) and CV death (death due to CV events) were analyzed.
Results
A total of 441,914 participants were enrolled (median age, 60 years; men, 57%). CV events and death occurred in 28.1% and 8.36% of the patients, respectively. The 10-year incidences of CV events and deaths increased from Q1 to 4. After adjusting for sex, age, income, type of diabetes drugs, comorbidities, and smoking and drinking status, the risk of CV events significantly increased according to the sequential order of the cost quartiles. In contrast, the risk of CV death showed a U-shaped pattern, which was the lowest in Q3 (hazard ratio [HR], 0.953; 95% confidence interval [CI], 0.913 to 0.995) and the highest in Q4 (HR, 1.266; 95% CI, 1.213 to 1.321).
Conclusion
Diabetes drug expenditure affects 10-year CV events and mortality. Therefore, affording an appropriate diabetes drug cost at a similar risk of CV is an independent protective factor against CV death. -
Citations
Citations to this article as recorded by- Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study
Tae Kyung Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Diabetology.2023;[Epub] CrossRef
- Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Improvement in Age at Mortality and Changes in Causes of Death in the Population with Diabetes: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
- Eugene Han, Sun Ok Song, Hye Soon Kim, Kang Ju Son, Sun Ha Jee, Bong-Soo Cha, Byung-Wan Lee
- Endocrinol Metab. 2022;37(3):466-474. Published online June 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1440
- 3,898 View
- 138 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Diabetes is a leading cause of death that is responsible for 1.6 million annual deaths worldwide. However, the life expectancy and age at death of people with diabetes have been a matter of debate.
Methods
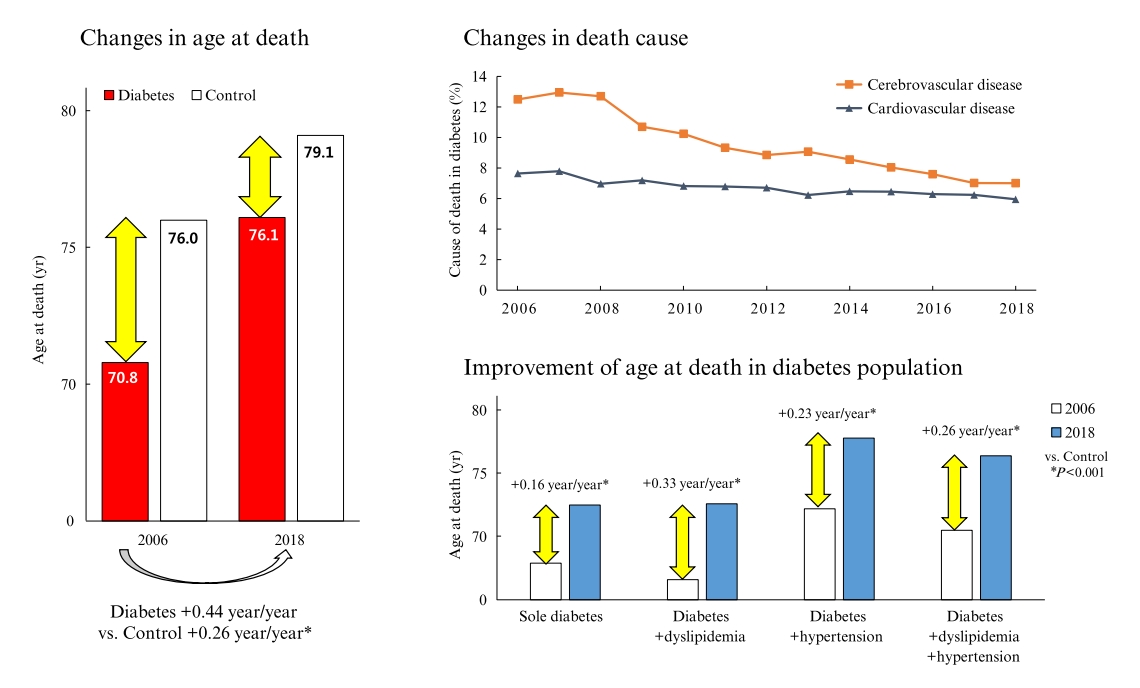
The National Health Insurance Service claims database, merged with death records from the National Statistical Information Service in Korea from 2006 to 2018, was analyzed.
Results
In total, 1,432,567 deaths were collected. The overall age at death increased by 0.44 and 0.26 year/year in the diabetes and control populations, respectively. The disparity in the mean age at death between the diabetes and control populations narrowed from 5.2 years in 2006 to 3.0 years in 2018 (p<0.001). In a subgroup analysis according to the presence of comorbid diseases, the number and proportion of deaths remained steady in the group with diabetes only, but steadily increased in the groups with diabetes combined with dyslipidemia and/or hypertension. Compared to the control population, the increase in the mean death age was higher in the population with diabetes. This trend was more prominent in the groups with dyslipidemia and/or hypertension than in the diabetes only group. Deaths from vascular disease and diabetes decreased, whereas deaths from cancer and pneumonia increased. The decline in the proportion of deaths from vascular disease was greater in the diabetes groups with hypertension and/or dyslipidemia than in the control population.
Conclusion
The age at death in the population with diabetes increased more steeply and reached a comparable level to those without diabetes. -
Citations
Citations to this article as recorded by- Analysis of Cause-of-Death Mortality in Children and Young Adults with Diabetes: A Nationwide 10-Year Follow-Up Cohort Study
Iee-Ho Choi, Sang-Woo Yeom, Sun-Young Kim, Jihye You, Jong-Seung Kim, Minsun Kim
Children.2023; 10(2): 358. CrossRef - Age at Mortality in Patients with Type 2 Diabetes Who Underwent Kidney Transplantation: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
Sun Ok Song, Eugene Han, Kang Ju Son, Bong-Soo Cha, Byung-Wan Lee
Journal of Clinical Medicine.2023; 12(9): 3160. CrossRef - Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(5): 525. CrossRef - Long-Term Cumulative Exposure to High γ-Glutamyl Transferase Levels and the Risk of Cardiovascular Disease: A Nationwide Population-Based Cohort Study
Han-Sang Baek, Bongseong Kim, Seung-Hwan Lee, Dong-Jun Lim, Hyuk-Sang Kwon, Sang-Ah Chang, Kyungdo Han, Jae-Seung Yun
Endocrinology and Metabolism.2023; 38(6): 770. CrossRef
- Analysis of Cause-of-Death Mortality in Children and Young Adults with Diabetes: A Nationwide 10-Year Follow-Up Cohort Study

- Clinical Characteristics of Patients with Adrenal Insufficiency in a General Hospital
- Ye Yeon Lee, Nan Hee Cho, Jong Won Lee, Nam Kyung Kim, Hye Soon Kim, Mi-Kyung Kim
- Endocrinol Metab. 2017;32(1):83-89. Published online February 28, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.1.83
- 4,460 View
- 60 Download
- 6 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Adrenal insufficiency (AI) is a life-threatening disorder caused by the deficiency of adrenal steroid hormones. This retrospective cross-sectional study investigated the characteristics of patients with AI in Korea.
Methods All consecutive patients with suspected AI who received care at a tertiary referral center in Korea in 2014 and underwent adrenocorticotropic hormone stimulation or insulin-tolerance testing were identified through a review of medical charts. Patients diagnosed with AI were enrolled. Their demographic, clinical, and treatment details were extracted.
Results Of 771 patients with suspected AI, 183 (23.7%) received a definitive diagnosis. The most common reason for testing was the presence of suspicious AI-related symptoms (30.0%), followed by a history of steroid medications (23.5%). Their mean age was 66.7 years, and females predominated (67.8%). The most common symptoms were general weakness, anorexia, arthralgia, and fever. Approximately half (53.6%) had a history of steroid use. Hydrocortisone was the most common treatment (71.6%), with most patients taking a 30 mg dose (44.2%). The most common dose frequency was twice a day (78.6%). Fourteen patients were treated for adrenal crisis (
n =10, 5.5%) or an intercurrent illness (n =4, 2.2%).Conclusion AI may have been caused by steroid medication use in many of the patients included in this study. The detection of AI can be improved by careful history-taking and being alert to the possibility that a patient has used steroids.
-
Citations
Citations to this article as recorded by- Risk of Mental Illnesses in Patients With Hypopituitarism: A Nationwide Population-Based Cohort Study
I-Hua Wei, Chih-Chia Huang
Psychiatry Investigation.2022; 19(6): 418. CrossRef - The Role of the Pharmacist in Optimizing Cancer Immunotherapy: A Retrospective Study of Nivolumab Adverse Events
Bradley D. Menz, Jacinta L. Johnson, Davina F. Gillard, William Chong, Michael B. Ward
Journal of Pharmacy Practice.2021; 34(3): 386. CrossRef - Clinical and biochemical factors to predict biochemical adrenal insufficiency in hospitalized patients with indeterminate cortisol levels: a retrospective study
Worapaka Manosroi, Natapong Kosachunhanan, Pichitchai Atthakomol
BMC Endocrine Disorders.2020;[Epub] CrossRef - Possible adrenal insufficiency among fatigue patients in a psychosomatic medical clinic
Sunao Matsubayashi, Nobuhiro Nakatake, Takeshi Hara
Endocrine Journal.2020; 67(1): 53. CrossRef - Encountering COVID-19 as Endocrinologists
Eun-Jung Rhee, Jung Hee Kim, Sun Joon Moon, Won-Young Lee
Endocrinology and Metabolism.2020; 35(2): 197. CrossRef - Glucocorticoid management of adrenal insufficiency in the United Kingdom: assessment using real-world data
Kamran Iqbal, Kate Halsby, Robert D Murray, Paul V Carroll, Robert Petermann
Endocrine Connections.2019; 8(1): 20. CrossRef
- Risk of Mental Illnesses in Patients With Hypopituitarism: A Nationwide Population-Based Cohort Study

- The Effect of Octreotide LAR on GH and TSH Co-Secreting Pituitary Adenoma.
- Nam Keong Kim, Yu Jin Hah, Ho Young Lee, Sang Jin Kim, Mi Kyung Kim, Keun Gyu Park, Ealmaan Kim, Hyukwon Chang, Hye Soon Kim
- Endocrinol Metab. 2010;25(4):378-381. Published online December 1, 2010
- DOI: https://doi.org/10.3803/EnM.2010.25.4.378
- 1,780 View
- 28 Download
-
 Abstract
Abstract
 PDF
PDF - Growth hormone (GH) and thyroid stimulating hormone (TSH)-secreting pituitary adenomas are very rare and they account for only 0.5% for all pituitary adenomas. These adenomas are usually treated with surgery, but this surgery is not easy because the tumor is usually huge and invasive. We reported here on a case of a GH-TSH-secreting adenoma in a 23-year-old male patient who was initially treated with octreotide LAR. He presented with symptoms of headache, palpitation and a visual defect that he had for the 3 months. He had hypertrophy of the frontal bone and enlargement of both the hands and feet. The visual field test showed bitemporal hemianopsia. The laboratory examinations showed high serum levels of free T4, TSH and free alpha-subunit. Additionally, the serum levels of GH and insulin-like growth factor-I (IGF-I) were increased. GH was not suppressed below 1microg/L by an oral 75g glucose loading test, and TSH was not stimulated by thyrotropin-releasing hormone (TRH). Because sellar MRI showed invasive macroadenoma encasing the vessels, we initially tried octreotide LAR for treatment. A year later, the IGF-I and thyroid function tests were normalized and the size of the tumor was reduced with cystic change. The symptoms of palpitation and headache were improved without a change of the visual field defect.

- Effects of Alpha-lipoic Acid on SREBP-1c Expression in HepG2 Cells.
- Tae Sung Yun, Ae Kyung Min, Nam Kyung Kim, Mi Kyung Kim, Ho Chan Cho, Hye Soon Kim, Jae Seok Hwang, Seong Yeol Ryu, Keun Gyu Park, In Kyu Lee
- J Korean Endocr Soc. 2008;23(1):27-34. Published online February 1, 2008
- DOI: https://doi.org/10.3803/jkes.2008.23.1.27
- 2,213 View
- 44 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Non-alcoholic fatty liver disease is common in patients with insulin resistance. Sterol regulatory element binding protein-1c (SREBP-1c) is a member of a family of transcription factors that have been recognized as key regulators for lipid accumulation in the liver that activate enzymes involved in the fatty acid biosynthetic pathway. This study was designed to evaluate whether alpha-lipoic acid (ALA) inhibits insulin-stimulated SREBP-1c expression. METHODS: We investigated the effects of ALA on insulin-stimulated SREBP-1c expression in a human hepatoma cell line (HepG2 cells) using Northern and Western blot analysis. We also examined the effect of ALA on the promoter activity of the SREBP-1c gene to examine whether ALA can affect SREBP-1c expression at the transcriptional level. To discern the mechanism by which ALA inhibits SREBP-1c expression, we examined the role of AMP-activated protein kinase (AMPK). RESULTS: Insulin increased the expression of SREBP-1c mRNA and protein in HepG2 cells in a dose depended manner. Co-treatment with ALA inhibited the insulin increased SREBP-1c expression in a dose-dependent manner. ALA also inhibited insulin-stimulated activation of the SREBP-1c promoter activity, indicating that ALA inhibited SREBP-1c expression at the transcriptional level. ALA increased phosphorylation of AMPK in HepG2 cells. Inhibition of the AMPK activity by compound C markedly reversed the inhibitory effects of ALA for insulin-stimulated SREBP-1c expression. These results suggest that ALA-induced suppression of SREBP-1c expression is at least in part mediated via AMPK activation. CONCLUSION: The present study suggests that ALA has an inhibitory effect on insulin-stimulated SREBP-1c expression. Therefore, further studies on the effects of ALA on hepatic steatosis in an animal model need to be performed. -
Citations
Citations to this article as recorded by- Effects of an aqueous extract of purple sweet potato on nonalcoholic fatty liver in high fat/cholesterol-fed mice
You Jin Lee, Yoon Kyoung Yang, You Jin Kim, Oran Kwon
Journal of Nutrition and Health.2015; 48(1): 1. CrossRef - Effects of an aqueous extract of purple sweet potato on nonalcoholic fatty liver in high fat/cholesterol-fed mice
You Jin Lee, Yoon Kyoung Yang, You Jin Kim, Oran Kwon
Journal of Nutrition and Health.2015; 48(1): 1. CrossRef
- Effects of an aqueous extract of purple sweet potato on nonalcoholic fatty liver in high fat/cholesterol-fed mice

- Association of Polymorphism in beta3-Adrenergic Receptor Gene with Fat Distribution.
- Tae Sung Yun, Yong Deuk Kim, Hye Soon Kim, Mi Jung Kim, Young Sung Suh, Jung Hyeok Kwon, Jin Soo Choi, Jung Guk Kim, Sung Woo Ha, Bo Wan Kim, Kyu Chang Won, Hyong Woo Lee, Ho Sang Shon, Ji Hyun Lee, Hyun Dae Yoon, Won Ho Kim, Young Gil Yun, In Kyu Lee
- J Korean Endocr Soc. 2003;18(2):184-192. Published online April 1, 2003
- 1,338 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Reasons for obesity include environmental factors and, more largely so, genetic factors. There have been many studies on these genetic factors. So far, genes related to obesity such as Leptin, Uncoupling Protein(UCP), Peroxisome proliferator activated receptor-gamma(PPAR-gamma), and Beta3-adrener-gic receptor(beta3-AR) gene have been discovered. Among these, beta3-AR is expressed in visceral adipose tissue and is thought to contribute to the regulation of resting metabolic rate and lipolysis. The missense mutation of beta3-AR gene, resulting in replacement of tryptophan by arginine at position 64(Trp64Arg), is associated with decreased resting metabolic rate and weightgain. We performed this study to determine if Trp64Arg polymorphism of beta3-AR gene is associatedwith obesity in Koreans. METHOD: We investigated the relationship between the beta3-AR gene mutation and body mass index (BMI), waist circumference, hip circumference, waist to hip ratio(WHR), area of subcutaneous fat, area of visceral fat, visceral to subcutaneous fat ratio(VSR), and lipid profile. 198 subjects were included in this study of which 97 were of normal weight and 101 were obese. Anthropometric data was obtained from physical examination and medical records. RESULT: In the cases of beta3-AR gene mutation of the obese group, the ratio of Trp/Arg and Arg/Arg are 43% and 5%, respectively, which were higher than the normal group(36%, 1%), although a statistical significant was not found. There was significant difference in the are of subcutaneous fat. Normal group(Trp/Trp) measured at 213.9+/-109.6cm2 versus 244.0+/-127.7cm2 (Trp/Arg) and 323.9+/-189.9cm2(Arg/Arg) for the mutation groups. Circumference of waist, circumference of hip, WHR, area of visceral fat, and VSR were higher in the mutation groups than in normal subject, but not significantly different. CONCLUSION: These results suggest that a genetic mutation in the beta3-AR gene can affect body fat composition, and is associated with obesity in Korean adults.


 KES
KES

 First
First Prev
Prev



